Part
01
of one
Part
01
Guest Profile - Dr. Jonathan Ripp
Key Takeaways
- Professor Jonathan Ripp is the Associate Dean for Well-being and Resilience and the Chief Wellness Officer at the Icahn School of Medicine at Mount Sinai (ISMMS). He is also a Professor of general internal medicine, medical education, as well as geriatrics and palliative medicine.
- PlumX Metrics reports that Professor Ripp has been recognized and invited as a participant in the Accreditation Council on Graduate Medical Education Symposia to speak on physician well-being. Further, it is reported that Professor Ripp was asked to not only join the American College of Physicians Promoting Physician Wellness Task Force, but he was also asked to take part in the National Academy of Medicine's Action Collaborative on Clinician Well-Being Resilience.
- Professor Ripp notes that his research and work has been based solely on the job burnout and well-being of physicians and the general medical fraternity. Mount Sinai reports that he has secured grants, lectured widely, and published several reports, articles, book chapters, reviews, and letters on the subject.
Introduction
Below, we detail a profile of Professor Jonathan Ripp that includes basic biographical information about his career, education, and active projects that he is currently involved in, affiliations, current work, and publications. The research team also attempted to curate a list of five potential questions about mental well-being in the medical industry, Professor Ripp's current work in that area, and his general expertise, that could a podcast host could ask him.
Biographical Information
- Professor Jonathan Ripp is the Associate Dean for Well-being and Resilience and the Chief Wellness Officer (CWO) at the Icahn School of Medicine at Mount Sinai (ISMMS). He is also a Professor of general internal medicine, medical education, as well as geriatrics and palliative medicine. As CWO, Mount Sinai's website notes, "Dr. Ripp oversees efforts to assess and provide direction for system- and individual-level interventions designed to improve well-being for all students, residents, fellows and faculty in the Mount Sinai Health System".
- He received both his undergraduate and medical degrees from Yale University (class of 2000), before joining Mount Sinai for a residency in internal medicine. Mount Sinai's profile states that Professor Ripp is "core faculty" in its Internal Medicine Residency Training Program and a valued member of the Mount Sinai Visiting Doctors home-based primary care program.
- He is also listed as the former Associate Dean of Graduate Medical Education at ISMMS, where he spearheaded well-being initiatives across the organization's training programs. Further, he is credited as co-founder and former director of ISMMS' Department of Medicine's Advancing Idealismion Medicine (AIM) initiative where he oversaw "a curriculum dedicated to the promotion of humanism and idealism in medicine".
- PlumX Metrics, an analytics company, also lists Professor Ripp as the Associate Director of the Arnhold Global Health Institute of the IMMS. The Institute "is dedicated to improving the health of under served communities worldwide through training and education of future leaders in Global Health practice and research".
Affiliations and Achievements/Accolades
- Professor Ripp is recognized as a leader in the field of physician and healthcare worker well-being by the medical community. PlumX Metrics reports that Professor Ripp has been recognized and invited as a participant in the Accreditation Council on Graduate Medical Education Symposia to speak on physician well-being. Further, it is reported that Professor Ripp was asked to not only join the American College of Physicians Promoting Physician Wellness Task Force, but he was also asked to take part in the National Academy of Medicine's Action Collaborative on Clinician Well-Being Resilience.
- He is affiliated with the Collaborative for Healing and Renewal in Medicine, or CHARM, a worldwide body he helped start and co-directs that comprises "medical educators, academic medical center leaders, experts in burnout research and interventions, and learners all working to promote learner and trainee wellness".
- According to his Mount Sinai profile, Professor Ripp is affiliated with the entire Mount Sinai Health System, which includes the Mount Sinai hospitals (main hospital, Morningwest, West, and Beth Israel), as well as the ISMMS.
- PlumX Metrics also reports that Professor Ripp has mentored and trained healthcare providers in rural Ethiopia and Brazil, while also led several service-based missions during the 2010 Haiti earthquake.
Current Work and Publications
- Professor Ripp notes that his research and work has been based solely on the job burnout and well-being of physicians and the general medical fraternity. Mount Sinai reports that he has secured grants, lectured widely, and published several reports, articles, book chapters, reviews, and letters on the subject.
- PlumX Metrics lists a total of 58 published works by Professor Ripp. Between 2020 and the time of this brief's publishing (19th August 2021), the website lists 14 publications. A full list can be viewed here.
- His 2020 article published in the American Medical Association's JAMA Network, Understanding and Addressing Sources of Anxiety Among Healthcare Professionals During the COVID-19 Pandemic, is his most cited and referenced work (according to PlumX Metrics data). This article posited 8 sources of anxiety/fears faced by front line healthcare workers. These fears include: "(1) access to appropriate personal protective equipment, (2) being exposed to COVID-19 at work and taking the infection home to their family, (3) not having rapid access to testing if they develop COVID-19 symptoms and concomitant fear of propagating infection at work, (4) uncertainty that their organization will support/take care of their personal and family needs if they develop infection, (5) access to childcare during increased work hours and school closures, (6) support for other personal and family needs as work hours and demands increase (food, hydration, lodging, transportation), (7) being able to provide competent medical care if deployed to a new area (eg, non-ICU nurses having to function as ICU nurses), and (8) lack of access to up-to-date information and communication". Together with fellow authors, Ripp argues that to effectively offer the required support, it is vital that healthcare systems and other relevant stakeholders understand these "specific sources of anxiety and fear".
- His latest 2021 publication dubbed "Psychological Impact of the COVID-19 Pandemic on Frontline Health Care Workers During the Pandemic Surge in New York City", looked into the possible psychological effects of the pandemic on healthcare workers. Ripp and fellow authors found that 39% of the healthcare workers interviewed admitted to experiencing symptoms of COVID-19 pandemic-related PTSD, major depressive disorders (MDD), or generalized anxiety disorder, or GAD.
- His mission at the Office of Well-Being and Resilience at ISMMS reads as follows, "to drive change by supporting initiatives that promote well-being and reconnect you with the meaning of your work". A key feature that underscores his work at the Office is narrated as follows, "One important feature of our model is the recognition that it is not incumbent on you as an individual to “get yourself well”. While we do encourage the development of your own individual resilience skills, we also recognize that much of what drives your well-being is located at the system-level".
Possible Podcast Questions
The following curated questions attempt to address Professor Ripp's achievements, work and research, state of mental well-being of medical practitioners, and the impact of the COVID-19 pandemic. The research team leveraged publicly available information on Professor Ripp's career, work and research, as well as current role as CWO, for inspiration.
- In the beginning of your career into the study of physician burnout and mental well-being, you started out by studying internal medicine resident physicians. What necessitated the shift to include other health care workers and possibly other members of the medical fraternity?
- In your 2020 article in the American Medical Association, Understanding and Addressing Sources of Anxiety Among Healthcare Professionals During the COVID-19 Pandemic, you highlighted 8 sources of anxiety that plagued healthcare workers. In the year and few months since its publication (also considering the surges in infections and new virus variants), have there been changes in the potency of these fears/sources of anxiety? Have some lessened/abated, morphed into different fears, or are they still valid fears held within the medical community?
- How has your role as Chief Wellness Officer shifted in response to the COVID-19 pandemic? What has been your most important ally and your biggest impediment in carrying out your role?
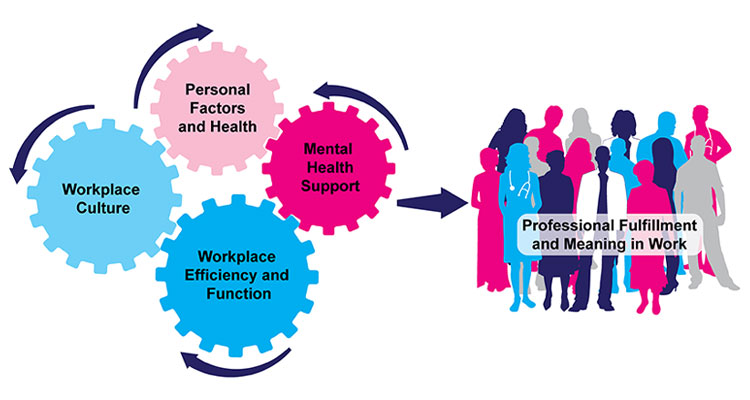
- The Office of Well-Being and Resilience that you head at Mount Sinai has a very detailed tool kit that details your organization's strategy on handling your front line healthcare professionals, trainees, faculty, and staff's mental well-being as well as addressing their most pressing concerns/fears. Could you elaborate on any successes and challenges you have had with both adopted models- the one that addresses the contributors to their professional fulfillment (pictured below) and the one crafted out of Maslow's Hierarchy of Needs? What insights would you give to other CWOs and healthcare systems looking to replicate what you have developed?
- What has your work and research taught you about healthcare workers' burnout and mental well-being? What surprised you the most? What has the medical industry overlooked and what steps can they take to effectively promote healthcare workers' mental wellness?
Research Strategy
For this research on Dr. Jonathan Ripp's profile, we leveraged the most reputable sources of information that were available in the public domain, including Mount Sinai websites (employee profiles and the Office of Well-Being web pages), JAMA network, Doximity, PlumX Metrics, and articles listed in the National Library of Medicine.
The curated questions were gleaned from these sources and attempted to address Professor Ripp's achievements, work and research, mental well-being in the medical industry, and the impact of the COVID-19 pandemic.