Part
01
of one
Part
01
Decline of Mental Health in the US
Research Strategy:
There are two parts to this research, based on client's goals. We divided our research into addressing mental health decline in the USA, and the rising burden of suicide in the USA. In covering mental health, we provided an overview of Americans who seek mental healthcare and identified the gaps in coverage. We also presented an outline of America's growing mental health crisis. In addition, we assessed presented how mental health is associated with suicide (covered in the suicide section). In the suicide section, we outlined incidence/prevalence statistics regarding suicide, a five-year trend of suicide rates (between 2013 to 2017), risk factors attributed to suicide, and the impact of legislation on suicide rates. Since the client focus is towards creating awareness and funding campaigns, we also highlighted various effective programs that have been implemented towards suicide prevention in the USA. If more research is required regarding preventive strategies and programs aimed at reducing suicide rates in America, a future meta-analysis can be provided that evaluates scientific studies and the degree of effectiveness.
MENTAL HEALTH:
Mental Health Service Use among American Adults:
- In 2018, around 37.1 million adults (age 18 or older) received mental healthcare during the past year.
- In 2018, nearly 47.6 million adults suffer from any mental illness (AMI); of which nearly 20.6 million (43.3%) received mental healthcare.
- The percentage of adults in 2018 with AMI who perceived an unmet need for mental health care in the past year was higher than the percentages in most years from 2008 to 2017.
- In 2018, about 2 out of 5 adults with AMI (45.2%) and slightly more than half of those (54.7 %) with any serious mental illness (SMI) who perceived an unmet need for mental health services did not receive services because they could not afford the cost of care.
- Over 85 million Americans live in areas with an insufficient number of mental health providers.
Mental Health Crisis in America:
- In America, the mental health crisis is prominent to the extent that for the first time in a century, life expectancies in the U.S have declined for three years in a row, which has largely been attributed to worsening mental health (as quoted by the article).
- In fact, the Affordable Care Act, along with other state and federal legislation, extended health insurance coverage to include mental health treatment.
- Lack of mental healthcare providers: Nearly 124 million people (approximately 40% of Americans) live in areas that face a shortage of mental health professionals. In fact, more than 60% of U.S. counties do not even have a single psychiatrist within their borders.
- A study investigated the prevalence of depression in the USA between 2005 to 2015, revealed a significant increase in depression from 8% to 13% (amongst age group 12-17 year-olds), and from 8% to 10.5% (amongst age group 18-25 year-olds). This research highlighted that the rate of increase in depression among youth was significantly more rapid relative to older groups.
- According to Mental Health America, key statistics related to the mental health 2020 report are outlined below:
- Youth Depression: In 2020, nearly 9.7% of youth in the U.S. suffer from severe major depression, in comparison to the 9.2% prevalence of depression in 2019.
- Rising Prevalence of mental illness: Prior to the pandemic (COVID-19), the prevalence of mental illness in adults was rising in the United States. In 2017-2018, at least 19% of adults experienced a mental illness - an increase of 1.5 million people from the 2016-2017 dataset.
- Unmet Need: Nearly 60% of youth with major depression did not receive any mental health treatment in 2017-2018. Even in states with the greatest access, over 38% are not receiving the mental health services they need. Among youth with severe depression, only 27.3% received consistent treatment. 23.6% of adults with a mental illness reported an unmet need for treatment in 2017-2018. This number has not declined since 2011.
- Uninsured Americans: In the U.S.A, approximately 10.8% are uninsured (5.1 million adults). These statistics vary across different states - New Jersey (ranked number 1) having 2.5% of adults with any mental illness (AMI) are uninsured, compared to Wyoming (ranked number 50) having 23% of adults with AMI are uninsured.
SUICIDE:
Background:
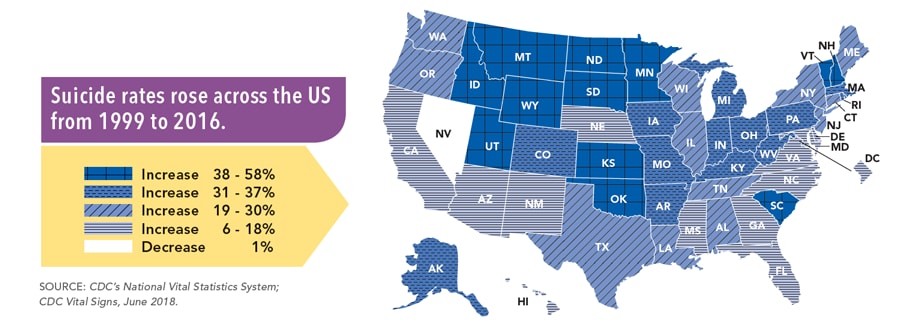
- Suicide ranks as the tenth leading cause of death in the United States. The suicide rates increase in nearly every state from 1999 to 2018.
- In 2018, nearly 48,344 lives were lost due to suicide (or intentional self-harm), resulting in about one death every 11 minutes.
- In 2018, 10.7 million American adults seriously thought about suicide, 3.3 million (4.3% adults) made a plan, and 1.4 million (0.6% adults) made a non-fatal suicide attempt.
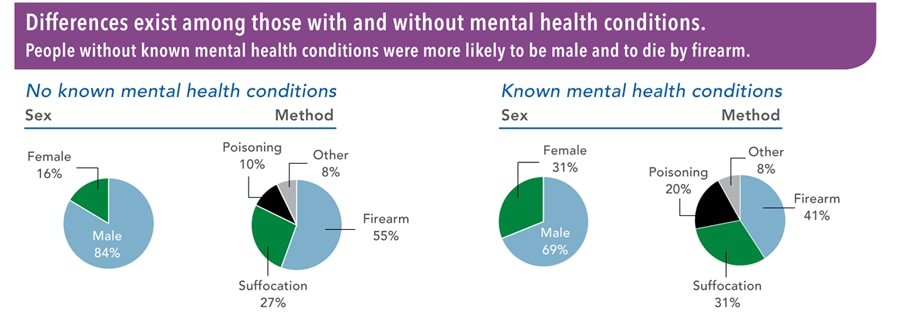
- Mental health conditions are often the cause of suicide, however, suicide is rarely attributed to any single factor. In fact, many individuals who die due to suicide are not known to have been diagnosed with mental health conditions at the time of their death.
- Etiological factors attributed to suicide include substance abuse, relationship issues, physical health, job, finances, legal, or housing stress.
- According to the CDC, nearly 45,000 lives were lost due to suicide in 2016.
- Suicide rates increased by 30% in nearly half of the states since 1999.
- Nearly 54% of individuals who died by suicide did not have a known mental health condition.
Suicide Incidence rates:
- A 5-year CDC'sdata for the age-adjusted death rate per 100,000 population, when adjusted for sex, race, Hispanic origin, and cause of death is highlighted here: 12.6 (2013), 13.0 (2014), 13.3 (2015), 13.5 (2016), 14.0 (2017) .
- The estimated number of deaths due to suicide (between 2013 to 2017) has been calculated as a product of incidence ratios and the total U.S. population in respective years as shown here: 39,690 (2013), 41,340 (2014), 42,560 (2015), 43,470 (2016), and 45,360 (2017).
Risk Factors Attributed to Suicide:
- According to the National Institute of Mental Health, the following major risk factors have been associated with suicide.
- Age between 15-24 years, and age greater than 60 years
- A prior suicide attempt
- Depression and other mental health disorders
- Substance abuse disorder
- Medical illness
- Family history of suicide
- Family history of mental health or substance abuse disorder
- Family history of violence (including physical or sexual abuse)
- Having guns or other firearms in the home
- Being in prison or jail
- Being exposed to others' suicidal behavior (such as family members, peers, or influential media figure)
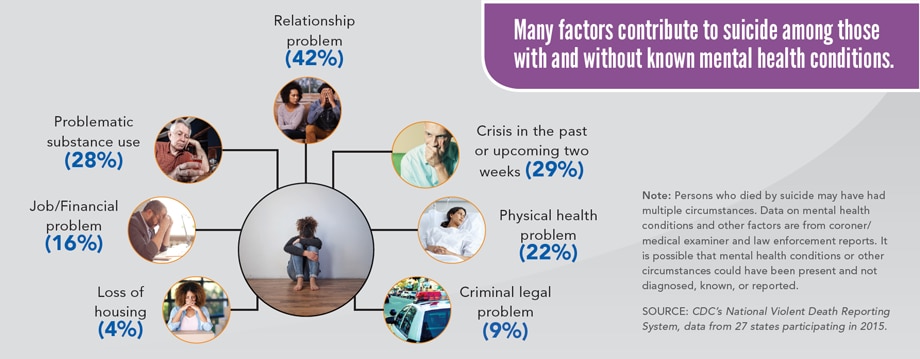
- According to the CDC's data from the National Violent Death Reporting System of 27 states (from 2015), have revealed factors contributing to suicide in individuals with and without known mental health conditions. Amongst which, the top three common reasons for suicide were having relationship problems (in 42% of cases), having a crisis in the past two weeks (in 29% of cases), and substance abuse (in 28% of cases).
Vulnerable Population:
- Other Risk Factors for suicide in vulnerable population - based on age group, culture, sexual orientation, occupation, and other demographic characteristics include:
- Stress resulting from prejudice and discrimination - a known risk factor for suicide attempts amongst LGBT youth. A study indicated that LGBTQ adolescents and adult males had a 4-times higher risk, while females had a two-times higher risk of suicide attempts when compared to heterosexuals.
- Research indicates that members of LGBTQ groups suffer from mental health problems, social isolation, misuse of alcohol and other drugs, and suicidal tendencies. The research also highlights ample evidence related to elevated suicide risk among the LGBTQ population compared to the heterosexual population.
- According to a recent survey (August 2020), that sampled over 40,000 LGBTQ youth members across ages 13-24 years in the USA, highlighted that nearly 40% of LGBTQ youth seriously considered suicide in the past year.
- Nearly 68% of LGBTQ youth reported symptoms such as generalized anxiety disorder in the past two weeks.
- Around 48% of LGBTQ youth reported engaging in self-harm in the past twelve months, including over 60% of transgender and nonbinary youth.
- 1 in every 3 LGBTQ youth reported that they had been physically threatened or harmed in their lifetime due to their LGBTQ identity.
- According to a CDC survey and other scientific studies, it has been reported that AI/AN communities experience an elevated suicide rate.
- The incidence of suicide in the AI/AN population, adjusted for age, sex, origin, and cause of death was 13.5 per 100,000 population (in 2017).
- High suicide rates amongst the AI/AN population is due to the historical trauma suffered as a result of resettlement, and the destruction of culture and economies.
- Numerous studies have shown that members of armed forces and veterans have also demonstrated a higher risk of suicidal tendencies due to heightened traumatic experiences faced during military service.
- In 2001, the Department of Defense (DoD) recorded a suicide incidence rate of 10.3 per 100,000 veterans; while in 2009, DoD reported a suicidal rate of 18.3 per 100,000 veterans.
- According to the CDC, veterans account for approximately 20% of suicidal deaths in America.
- Drug overdose and the misuse of prescription medication were the most frequent methods for suicide attempts in the given population.
- According to another study, nearly half of all suicides in the Veteran Health Affairs occurred amongst veterans with known mental health conditions.
- For suicide prevention in veterans, reach out to the suicide prevention lifeline organization.
LGBT population:
American Indian/Alaskan Natives (AI/AN):
Veterans:
Suicide and Mental Health amongst Vulnerable Population (LGBTQ members):
- Based on a recent cross-sectional study (The Trevor Project) that investigated the association between worsening mental health and suicide rates amongst the LGBTQ population, published the findings shown below. This study was by far the largest survey conducted on the given population (40,000 respondents across the USA).
- One of the key findings was that amongst 40,000 respondents, 21% of age 13-17 years, and 10% of 18-24 years old have attempted suicide. In comparison, nearly 48% of age 13-17-year-olds, and 34% of 18-24 years old have considered suicide.
Impact of Legislation on Suicide Rates:
- According to a study (Harris K et al., 2006) has found that 12 months after the states enacted the 'mental health parity laws,' the self-reported use of mental healthcare services significantly increased (by 1.2 percentage points).
- Another study (Lang M, 2013) investigated the impact of parity laws on suicide rates between 1990 and 2004. The study indicated that improved legislation regarding mental health parity laws was associated with a 5% decrease in the suicide rate, which is equivalent to preventing 592 suicides per year (in 29 states).
Suicide Prevention Strategies/Programs:
- According to the Suicide Prevention Resource Center, the protective factors against suicide include:
- Effective Behavioral healthcare
- Connectedness to individuals, family, community, and social institutions
- Life Skills (include critical thinking, stress management, problem-solving, and conflict resolution and coping skills)
- Sense of Purpose in life
- Religious/Cultural/Personal beliefs that discourage suicide.
Mental Health Disorders and Suicide:
- Mental and Substance-abuse disorders are recognized as important risk factors for suicidal behaviors across all age groups. Mental disorders such as (i) mood disorders, (ii) anxiety disorders, (iii) borderline personality disorder, and (iv) schizophrenia increases the likelihood of suicidal risk.
- Includes individuals suffering from major depressive disorder (or unipolar disorder) may become a life-threatening psychiatric illness.
- Bipolar disorder - more than 60% of suicidal deaths occur in patients with mood disorders; while 80% of patients with bipolar disorder have suicidal ideation plus suicidal attempts.
- Anxiety disorder - affecting nearly 40 million Americans (age 18 and older). These disorders can be characterized as phobia, panic disorder, agoraphobia, PTSD, and obsessive-compulsive disorder. The presence of any anxiety disorder has been significantly associated with suicidal ideation and suicidal attempts.
- Borderline Personality disorder (BPD) - characterized as an emotional disorder with pervasive patterns of instability in interpersonal relationships, self-image, and emotions. It has been reported that 3-10% of patients with BPD die with suicide.
- Schizophrenia - characterized by disturbances in perception, thought, language, and social function. A meta-analysis of 60 studies identified that almost 5% of schizophrenic patients die by suicide.
- According to the CDC, Alcohol, and drug-abuse rank second to depression and mood disorders as the most frequent risk factors for suicide. In fact, According to data from the National Violent Death Reporting System (NVDRS), in 2007, alcohol was a factor in nearly one-third of reported suicides.
- In 2018, 3.6% of the American population misused prescription pain-relieving medications, as the second most common form of illicit drug use.
- In 2018, the substances with the largest number of recent (i.e., past year) initiates of use or misuse were alcohol (4.9 million new users), marijuana (3.1 million new users) prescription pain relievers (1.9 million new misusers), and cigarettes (1.8 million new users).
- For further reading, access CDC material here.